
Variant anti-FIXa arms (identified by symbol and color coding as in panel D) were assembled with the parental anti-FX arm. (E) Plasma activity of a representative subset of biAbs from cycles of anti-FIXa arm optimization.

A total of 1308 variants were investigated, with the distribution of activities within each round shown as a violin plot. FIXa stimulation was measured in high throughput at pH 7.4 in the presence of 0.15 to 1 nM FIXa, 100 nM FX, 500 µM PS:PC vesicles, and a single concentration (800 nM) of anti-FIXa OA. (D) Evolution of FIXa stimulation of variants of the parental Mim8 anti-FIXa arm during rounds of mutational optimization. Complementarity-determining region (CDR) loops are highlighted in gray. (C) Number of unique amino acid substitutions explored at individual positions (using consecutive numbering) in the heavy (V H) and light (V L) chain variable domains of the Mim8 anti-FIXa arm. Assays used to investigate functional, structural, and biophysical properties of biAb, anti-FIXa OA, and mAb variants are indicated. An overview of the pursued mechanism of action of Mim8 (A) and screening and optimization strategy (B) is shown. High-throughput screening for FVIIIa-mimetic activity. 8 With this in mind, the current study aimed to design a highly potent and efficacious FVIIIa-mimetic antibody. 5,6 Even though both FVIIIa and FVIIIa-mimetics stimulate FIXa-mediated activation of FX, there are differences in their modes of action, 7 and the cofactor activity of FVIIIa is considerably greater than that of emicizumab. Emicizumab mimics the effect of FVIIIa by binding to activated factor IX (FIXa) and factor X (FX), 4 and it has exhibited good efficacy for prophylactic treatment of HA patients with or without inhibitors. 3 With the launch of the activated FVIII (FVIIIa)-mimetic bispecific antibody (biAb) emicizumab (Hemlibra ), the first subcutaneous (SC) prophylactic treatment became available. Likewise, until recently, the bypassing agents available for the treatment of HA patients with inhibitors have been intravenously administered products (recombinant activated FVII and activated prothrombin complex concentrate) and with limited options available for prophylactic therapy due to their short half-lives in circulation. 1 However, a serious complication of FVIII treatment of HA is the development of neutralizing antibodies (inhibitors) in ∼30% of patients, 2 as well as the risk and inconvenience associated with intravenous (IV) administration. Recombinant factor VIII (FVIII) molecules have eliminated the risk of viral transmission, and extended half-life FVIII products have further reduced the treatment burden of prophylaxis. Treatment options for people with hemophilia A (HA) have for the past 2 decades improved markedly. In conclusion, Mim8 is an activated FVIII mimetic with a potent and efficacious hemostatic effect based on preclinical data. Furthermore, the pharmacokinetic parameters of Mim8 were investigated and a half-life of 14 days shown in cynomolgus monkeys. A similar potency difference was observed in a tail vein transection model in hemophilia A mice, whereas reduction of bleeding in a severe tail-clip model was observed only for Mim8. In hemophilia A plasma and whole blood, Mim8 normalized thrombin generation and clot formation, with potencies 13 and 18 times higher than a sequence-identical analogue of emicizumab. In addition, the activity of Mim8 was dependent on stimulatory activity contributed by the anti-FIXa arm, which enhanced the proteolytic activity of FIXa by 4 orders of magnitude. Binding affinity with FIXa and FX in solution was much lower, with equilibrium dissociation constant values for FIXa and FX of 2.3 and 1.5 µM, respectively. The resulting bispecific antibody (Mim8) assembled efficiently with FIXa and FX on membranes, and supported activation with an apparent equilibrium dissociation constant of 16 nM.
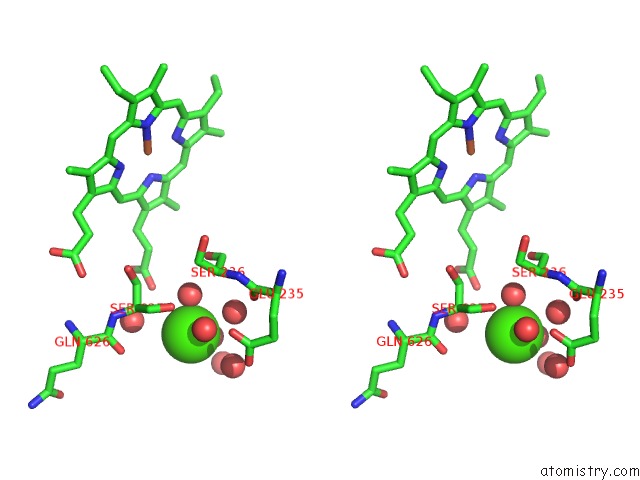
To mimic this property in a bispecific antibody format, a screening was conducted to identify functional pairs of anti-FIXa and anti-FX antibodies, followed by optimization of functional and biophysical properties. Hemophilia A is a bleeding disorder resulting from deficient factor VIII (FVIII), which normally functions as a cofactor to activated factor IX (FIXa) that facilitates activation of factor X (FX).


 0 kommentar(er)
0 kommentar(er)
